Antibiotics, the miraculous drugs that revolutionized medicine in the 20th century, are rapidly losing their power. However, a forgotten treatment, discovered over a century ago, offers hope.
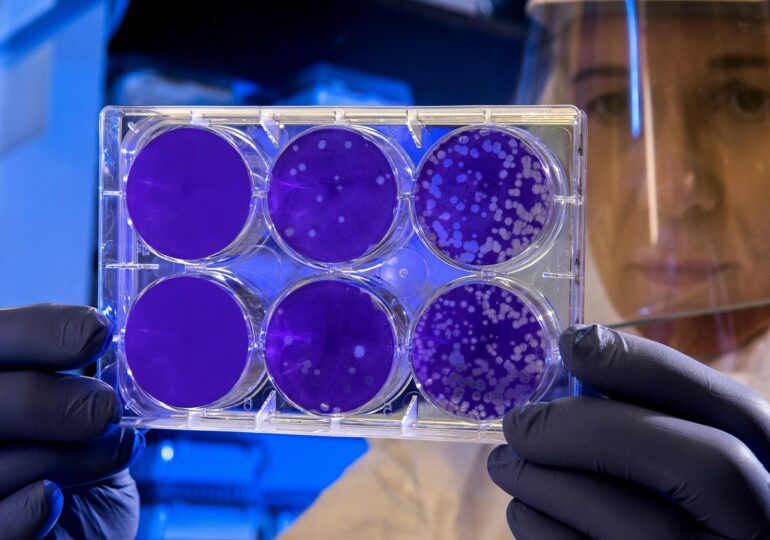
By 2050, drug-resistant „superbugs” could kill up to 10 million people per year, according to the World Health Organization (WHO). Phage therapy could help us avoid this scenario. It uses viruses that naturally feed on bacteria, diverting and destroying them from the inside out, as reported by Newsweek.
A new study published in Cell Reports has found that bacteria can use a survival trick when attacked by viruses. Instead of letting the infection spread, the bacteria create a kind of internal "quarantine zone" around the virus, isolating it from the rest of the cell. Deprived of resources, the virus cannot multiply and dies.
In Search of a Method to Neutralize Bacterial Defense
Scientists from the University of Melbourne and the Hebrew University of Jerusalem discovered this process after conducting genetic experiments and using powerful imaging tools that can magnify cells in 3D. This allowed them to observe, almost in real-time, how bacteria fought the invading virus.
"We found that attacked bacteria can divide asymmetrically, so they can exclude the infected part and save the rest of the cell," said the study's author and microbiology professor Sigal Ben-Yehuda to the cited publication.
Understanding how this mechanism works is an essential first step in discovering a method of neutralization to make therapy more effective, the researchers explained.
One approach could involve, for example, adding a special compound that would prevent the bacterial sensor protein from detecting the intruder.
Phage therapy can be used in various ways in medicine, depending on the nature of the infection. Approaches studied or already used in a limited manner include pills and liquids, topical creams, sprays or bandages, and intravenous injections.
Last year, phage therapy helped save a pet cat named Squeaks after developing a multi-drug-resistant infection and after months of failed antibiotic treatment.
Veterinarians in Israel used a carefully tailored mix of bacteria applied directly to the cat's paw wound, alongside antibiotics that no longer worked alone. Within a few weeks, the infection cleared, and the surgical site healed. This was the first documented use of personalized therapy on animals.
Antibiotics No Longer Help Us
For nearly a century, antibiotics have been a cornerstone remedy for combating bacteria. However, bacteria are becoming increasingly resistant to antibiotics.
The use of antibiotics has increased by over 21% since 2016, and a recent study by the Global Research on Antimicrobial Resistance (GRAM) Project, published in The Lancet, found that over a million people die each year due to antimicrobial resistance, which includes resistance to antibiotics, antifungals, antiparasitics, and antivirals.
Phage therapy is still considered an experimental approach in much of the Western world, although it has been used for decades in countries like Georgia and Poland.
These new discoveries provide a fresh impetus in this area of research, offering hope that in the future, phage therapy could be added to treatment methods or even replace antibiotics in curing persistent infections.
T.D.